Select the audit that matches the number of patients you plan to enrol.
Note: you can't swap between audits, once you start one audit, you need to complete that audit before any CPD hours will be allocated.
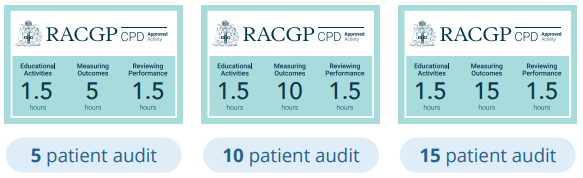
This is a flexi-audit where GPs may choose to consult 5, 10 or 15 patients. Duration depends on number of patients enrolled.
15 patient audit - 18 CPD hours
10 patient audit - 13 CPD hours
5 patient audit - 8 CPD hours
Regardless of whether you enrol in the 5, 10 or 15 patient audit, this education is designed to take place over multiple weeks. It cannot be completed in one sitting. You can stop at any time, and progress will be saved. Education you have started can be found on your Dashboard.
CPD hours for each option:
On any given day in Australia, about 53,000 people are receiving pharmacotherapy treatment for opioid dependence.1 In 2023, more patients received a buprenorphine formulation than methadone for the first time.1
This clinical audit begins with a 1.5-hour pre-learning activity exploring case studies in opioid use disorder, current options for opioid dependency treatment, and the use of opioid pharmacotherapies in medication assisted treatment of opioid dependence (MATOD). Risks and benefits of latest opioid agonist treatments will be covered, with a focus on long-acting injectable buprenorphine (LAIB) products.
After completing the pre-learning activity, GPs will perform a clinical audit of 5, 10 or 15 patients currently receiving MATOD in the form of sublingual buprenorphine, or methadone. Patient management will be reviewed against Australian ODT guidelines, and GPs will assess whether the patient could benefit from switching to a long-acting injectable buprenorphine (LAIB) medication. Guidance is provided on how to undertake this switch, either in the primary care setting or with appropriate referral for specialist care.
Patient eligibility criteria for this clinical audit:
- Adult patients, 18 years or over
- Currently receiving maintenance ODT with one of the following:
- Methadone oral liquid (Aspen Methadone Syrup, Biodone Forte)
- Buprenorphine sublingual (SL) tablet (Subutex)
- Buprenorphine + naloxone fixed dose combination (Suboxone Film)
- No known contraindications to treatment with LAIB are present.*
*Contraindications to all LAIB products: Hypersensitivity to buprenorphine or to any of the excipients in the product, severe respiratory insufficiency, severe hepatic insufficiency (Child-Pugh C),
Additional contraindications to Sublocade: Subject <18 years of age, acute intoxication with alcohol or other CNS depressants. Additional contraindications to Buvidal Weekly and Monthly: Subject <16 years of age, acute alcoholism or delirium tremens.
You must select at least one patient undergoing treatment with SL BUP (with or without naloxone) and at least one patient receiving treatment with methadone.
- Australian Institute of Health and Welfare (2024) National Opioid Pharmacotherapy Statistics Annual Data collection, AIHW, Australian Government, accessed 17 December 2024.






